The Recipe to a Healthy Heart:Your Guide to Preventing Heart Disease
Sure, the taste of food is important, but do you know how your diet impacts your heart? Many foods contain hidden ingredients that negatively impact...

There are clear links between mental health and heart health — research increasingly shows that stress is a significant factor that contributes to coronary heart disease risk.
For decades, doctors and health institutions have recommended monitoring risk factors for cardiovascular disease linked to physical health. These include high cholesterol, physical inactivity, smoking, and alcohol consumption.
While all of these do play a role in heart health and overall health, there’s one thing missing. Research increasingly shows that stress is a significant factor that contributes to coronary heart disease risk. Increased stress can also increase the prevalence and severity of risk factors such as hypertension (high blood pressure), obesity, and Type 2 diabetes.1,2
In other words, there are clear links between mental health and heart health – and clear benefits to reducing everyday stress and anxiety wherever possible.
In 2004, the INTERHEART study concluded that psychosocial factors such as stress were “significantly related to acute myocardial infarction,” the medical term for a heart attack. Researchers determined that stress was an independent risk factor. It wasn’t directly related to more well-documented risk factors such as high cholesterol or blood pressure, smoking status, alcohol consumption, diet, or physical activity; it also wasn’t linked to patients’ demography or geography.3
Subsequent research has solidified the connection between stress and heart disease. A 2020 paper summarized several imaging studies showing how the body’s hormonal, behavioral, and involuntary responses to stress may cause arterial inflammation or arterial hardening, increases the production of white blood cells, and may require the heart to work harder to pump.1 Shortly after, a 2021 study found that stress “was significantly associated with an increased risk of cardiovascular death or nonfatal myocardial infarction” in patients who had been diagnosed with coronary heart disease.2
“While not part of most [cardiovascular disease] treatment guidelines, it may be appropriate to address stress in individuals at risk for CVD given the low cost and low risk of intervention,” the 2020 paper concluded. “Beyond encouraging treatment of underlying stress disorders, cardiologists should be aware of the impact of chronic stress on patients’ health.”
To properly address, manage, and potentially reduce stress, it’s important to understand that different kinds of stress impact heart health differently.1, 4, 5
It’s worth noting that small amounts of stress can be beneficial. Feeling a knot in the stomach because a deadline is approaching may encourage someone to complete a task, while jumping at a loud noise may help someone avoid an accident. But it’s also clear that too much stress, especially chronic stress, may affect heart health and increase risk of cardiovascular disease.
Too often individuals may experience chronic stress without realizing the toll it is taking on their mental and physical wellbeing. One way to identify whether your own stress is particularly high is through a Perceived Stress Score (PSS).A
PSS can be identified by completing a ten-item questionnaire that asks how often certain feelings of stress have occurred in the past month. Your final score from the questionnaire can give you an idea if your perceived stress is low, moderate or high. This test was created by researchers in 1983 and remains a popular way to help diagnose chronic stress.6
Knowing how to manage stress is critical to reducing its potential impact on heart health. These tips from the American Heart Association and Centers for Disease Control and Prevention may help.5, 7
Because different types of stress have different causes, not every technique for reducing stress will work every time. It may take some time to figure out which stress management techniques are most effective. In situations where individuals may not be able to remove or otherwise directly address causes of chronic or psychosocial stress, management techniques may require modification to better fit the situation.
Stress is a part of everyone’s life. It’s important to recognize when it’s helpful and when it’s harmful – and how that harm can be bad for the heart.
Recognizing how you typically cope with stress in your life can be the first important step to creating more mindful, heart-healthy habits. However, if stress feels overwhelming, reach out to a mental health professional who can help you find a strategy that provides relief. Learning how to reduce stress has many mental and physical benefits, and all it may take is a few simple actions every day.
Cleerly was founded on the mission to create a world without heart attacks. Our AI-enabled software simplifies heart scans into easily understood reports that both doctors and patients can use to define coronary artery disease risk. To learn more about how Cleerly is changing the paradigm of heart care and improving heart attack prevention, subscribe to our newsletter.
References:
1. Disentangling the Links Between Psychosocial Stress and Cardiovascular Disease ⇱ Circulation: Cardiovascular Imaging. August 2020.
2. Association of Mental Stress–Induced Myocardial Ischemia With Cardiovascular Events in Patients With Coronary Heart Disease. ⇱ Journal of the American Medical Association. November 2021.
3. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. ⇱ Lancet. September 2004.
4. The Three Types of Stress ⇱ Psychology Today. December 2018.
5. Chronic Stress Can Cause Heart Trouble ⇱ American Heart Association. February 2020.
6. A Global Measure of Perceived Stress ⇱ Health Soc Behav. 1983.
7. Reduce Stress in 10 Minutes and Improve Your Well-Being ⇱ Centers for Disease Control and Prevention. 2022.

Sure, the taste of food is important, but do you know how your diet impacts your heart? Many foods contain hidden ingredients that negatively impact...
As we reach the end of 2023 and yet another remarkable year at Cleerly, it’s a great opportunity to reflect on all we’ve accomplished and begin...

Cleerly has had a busy few months – attending conferences, panel sessions, and winning awards as we all work together to achieve our mission of a...

Half of patients who have a heart attack don't show symptoms prior to their event. A new standard of precision care, emphasizing comprehensive...

Sure, the taste of food is important, but do you know how your diet impacts your heart? Many foods contain hidden ingredients that negatively impact...
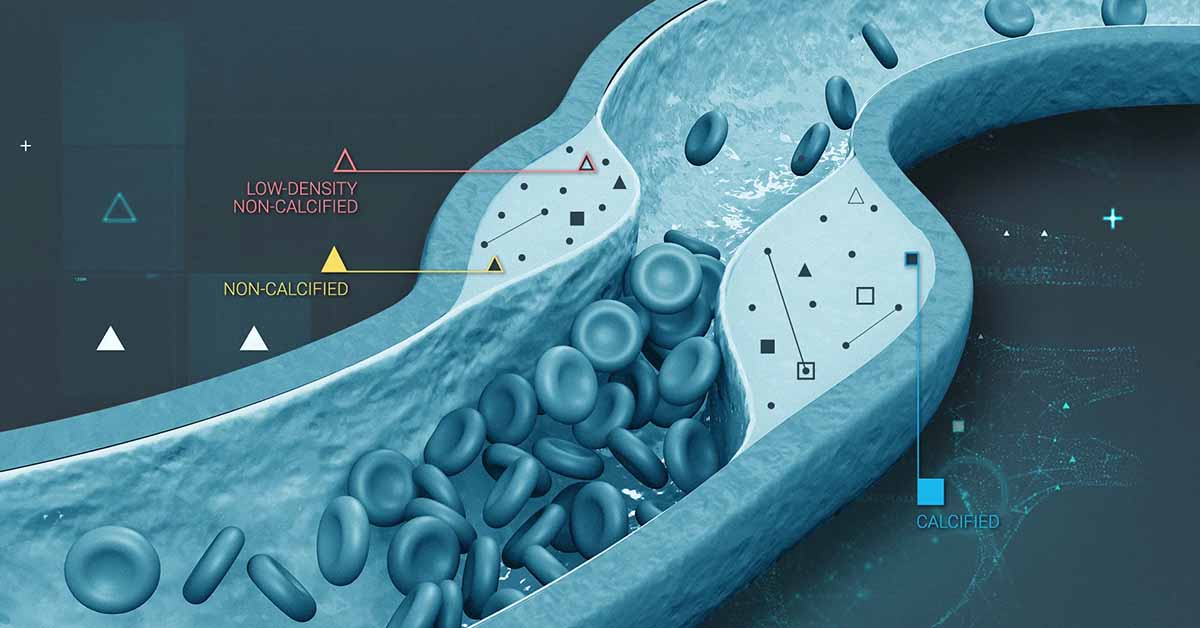
Heart plaques, which are the build-up of substances like cholesterol and fat in the heart’s arteries, can increase your risk of heart attack. A...